Description of the procedure
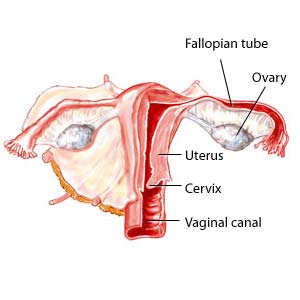
An oophorectomy is a surgical procedure to remove one or both ovaries. Oophorectomy may also be used to remove part of an ovary. The ovaries produce eggs as well as the hormones estrogen and progesterone.
Removal of one ovary still allows a woman to continue to menstruate and to have children, as long as the remaining ovary is not damaged. When both ovaries are removed, menstrual periods stop, a woman can no longer become pregnant, and estrogen and progesterone are no longer produced by the reproductive system.
During an oophorectomy, other surgical procedures such as a hysterectomy (removal of the uterus) or removal of the fallopian tubes may also be performed.
Doctors perform this procedure in a hospital under general anesthetic.
When should this procedure be performed?
Doctors perform this procedure as required to remove either one or both ovaries.
Why is this procedure performed?
The main reason for an oophorectomy is to treat problems related to a woman's reproductive organs. Cancer of one or both of the ovaries, prevention of ovarian cancer, and removal of ovarian cysts or abscesses may also require a woman to have an oophorectomy. It may also be required if you have an ovarian torsion (twisting of an ovary), which can lead to sharp lower abdominal pain.
An oophorectomy may also be needed if a woman has a type of cancer that is stimulated by estrogen. Breast cancer may be treated with an oophorectomy or it may reduce a woman's risk of developing breast cancer. Removing one or both ovaries reduces the body's estrogen level in these cases.
Severe cases of endometriosis can also be treated with this procedure to reduce estrogen levels.
Are there any risks and precautions?
Certain risks are common to all surgery and anesthesia. These risks depend on many factors including the type of surgery and your own medical condition. The possible, but very rare, side effects include: side effects of the anesthetic, breathing problems, infection, bleeding, scarring, and death.
Although oophorectomy is generally considered safe, it does have some risk of side effects or complications. These include:
- damage to nearby organs during the procedure
- blood clots
- bleeding
- changes in sex drive
- depression
- infection
- premature menopause (if both ovaries are removed)
- rupture of a tumour, which can lead to the spreading of cancerous cells
- continued signs and symptoms (e.g., lower abdominal pain) due to leftover ovary cells (this is called ovarian remnant syndrome)
If you experience any of these side effects or complications, contact your doctor immediately.
If you are concerned about any symptoms following this procedure, speak to your doctor. Take the time to be sure you understand all the risks of complications and side effects as well as any precautions you or your doctor can take to avoid them. Be sure your doctor understands all your concerns.
What happens during the procedure?
There are two methods for performing this procedure. Both are done under general anesthesia so you will not be awake.
In the first method, the doctor makes an incision in the abdomen below the belly button. The doctor locates the ovaries below the abdominal muscles. One or both ovaries (or parts of the ovaries) are then removed. The fallopian tubes may be removed at this time as well.
In the second method, a small incision is made in the navel (belly button) and a laparoscope is inserted. A laparoscope is a thin tube with a camera and light on the end so the doctor can see the area. Other instruments are used to cut and remove one or both ovaries (or parts of the ovaries).
The procedure usually lasts about 1 to 4 hours.
How should I prepare for this procedure?
Before having this procedure, discuss with your doctor the advantages, disadvantages, long-term risks, and consequences associated with the procedure. Be sure you fully understand what will happen and are comfortable with your doctor's answers to your questions. If you want to have children, talk to your doctor about your options.
Your doctor may request tests such as an ultrasound or X-rays before the surgery. These images allow the doctor to see the area before the procedure. Your doctor may also request other tests (e.g., blood or urine tests). A laxative or enema may be recommended if extensive surgery is anticipated, to clean out the colon.
Do not eat for 8 hours before the procedure. You may be able to drink clear liquids until 2 hours before the procedure. If your doctor has recommended different times, follow the timing recommended by your doctor.
Tell your doctor or prescriber about all prescription, over-the-counter (non-prescription), and herbal medications that you are taking. Also tell them about any medication allergies and medical conditions that you may have. Arrange for someone to drive you home from the hospital.
Ask your doctor or pharmacist whether you need to stop taking any of your medications before the procedure.
What can I expect after the procedure?
The standard procedure following surgery with general anesthetic will be followed.
- Immediately after surgery, you will be brought to the hospital’s recovery room until the anesthetic wears off. Nurses will be available if you need help. You will likely feel groggy, sore and possible nauseated.
- After you have recovered from the anesthetic you will be transferred to a hospital ward for the rest of your hospital stay, if you are staying over night. If you are not staying over night, you will be discharged from the hospital and allowed to go home.
- Before you go home, the doctor or nurse will go over what you need to do at home to complete your recovery.
It is common for women to stay in the hospital for 2 to 5 days after the oophorectomy using the abdominal incision method. Women who underwent an oophorectomy using a laparoscope may be discharged earlier.
It will take 2 to 6 weeks to recover from the procedure. Recovery time may be longer if it is part of a hysterectomy (surgical removal of the uterus). Pain and discomfort are normal after the procedure. Medication can be used to ease the pain.
Antibiotics are often recommended to help reduce the risk of infection.
Women who have both ovaries removed may need to take hormones if they are not already going through menopause and do not have cancer. Hormone therapy (HT) reduces the symptoms associated with menopause caused by the rapid decrease of estrogen in the body. But HT is not for everyone - talk to your doctor about whether this treatment is appropriate for you.
Changes in a woman's body may affect her emotionally and psychologically. A decrease in estrogen often leads to a decline in sexual desire. Getting support from health care professionals and talking to others who have had the procedure can improve a person's well-being during recovery.
Results
The results will vary depending on the reason for the oophorectomy. Oophorectomy is an effective treatment and prevention method for ovarian cancer and some types of breast cancer. It can also relieve the symptoms of ovary-related problems such as cysts and abscesses.
All material copyright MediResource Inc. 1996 – 2024. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/procedure/getprocedure/Ovary-Removal